Bouts of disabling pain, bleeding, weight loss and hospitalization that sometimes require surgery: that's the lot of about three million adults in the U.S. who suffer from inflammatory bowel disease, or IBD. (The illness has two main forms, Crohn's disease and ulcerative colitis. It is frequently associated with an overactive immune system and may have a genetic component.) Treatments often involve some variety of immunosuppressant such as a steroid drug. But even controlled cases have periodic flare-ups, and the reasons have been hard to pin down.
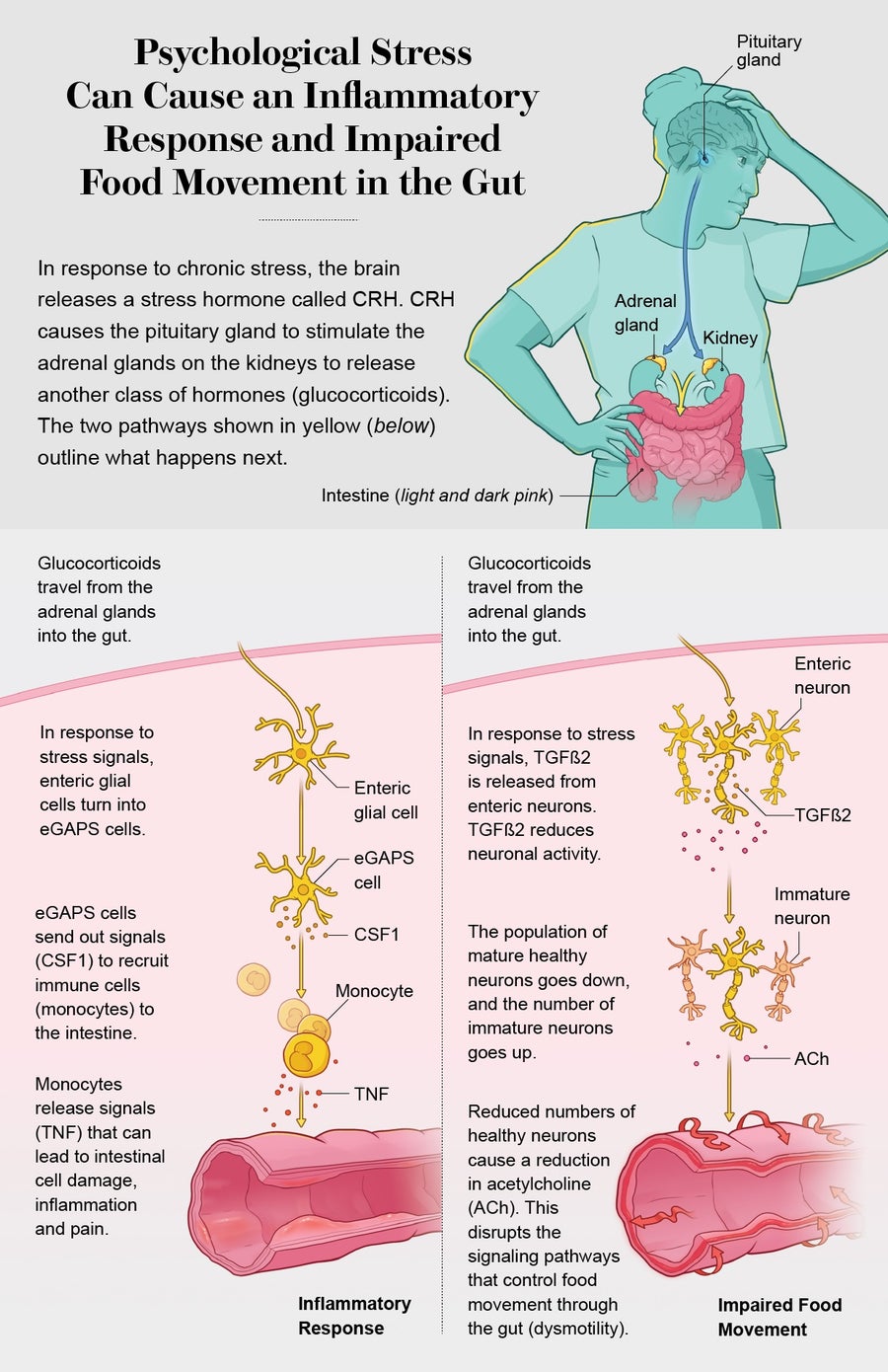
Now scientists have traced two detailed molecular pathways from the brain to the gut that produce IBD flares. And in three different groups of IBD patients, they found that psychological stress—a death in the family or a bad fight with a loved one, for instance—can trigger the release of brain chemicals that cause IBD symptoms. This doesn't mean IBD is all in the head, emphasizes Christoph A. Thaiss of the University of Pennsylvania, one of the researchers. But it does mean psychotherapy and targeted stress-management techniques have important—and until now underappreciated—roles to play in preventing and treating agonizing flares.