Liz Williams was standing pitchside at a women’s rugby match, and she did not like what she was seeing. Williams, who researches forensic biomechanics at Swansea University, UK, had equipped some of the players with a mouthguard that contained a sensor to measure the speed of head movement. She wanted to understand more about head injuries in the brutal sport. “There were a few instances when my blood went cold,” Williams said.
When the women fell in a tackle, their heads would often whiplash into the ground. The sensors showed that the skull was accelerating—indicating an increased risk of brain injury. But medical staff at the match, not trained to look out for this type of head movement as a cause of injury, deemed the women fine to play on. Such whiplash injuries are much rarer when males play.
Williams’ observations highlight an increasingly apparent problem. A growing body of data suggests that female athletes are at significantly greater risk of a traumatic brain injury event than male athletes. They also fare worse after a concussion and take longer to recover. As researchers gather more data, the picture becomes steadily more alarming.
Female athletes are speaking out about their own experiences, including Sue Lopez, the United Kingdom’s first semi-professional female football player in the 1970s, who now has dementia—a diagnosis she has linked to concussions from heading the ball.
Researchers have offered some explanations for the greater risk to women, although the science is at an early stage. Their ideas range from differences in the microstructure of the brain to the influence of hormones, coaching regimes, players’ level of experience and the management of injuries.
Given that most, if not all, sports-concussion protocols are based on data from men, female athletes ranging from schoolgirls to this year’s Olympic football squads are being put at risk of serious injury. “We take all of these data, primarily from studies on men; we apply them to women. That’s just got to change,” says Michael Grey, who researches rehabilitation neuroscience at the University of East Anglia in Norwich, UK.
Head injuries in sport have had a high profile for many years, with hundreds, if not thousands, of participants in American football, rugby, football, boxing and other sports experiencing dementia or memory loss thought to be linked to recurrent blows to the head decades earlier. Coaching protocols at all levels are changing to try to prevent injury, but these have generally neglected to include a huge cohort: women.
Bigger risk
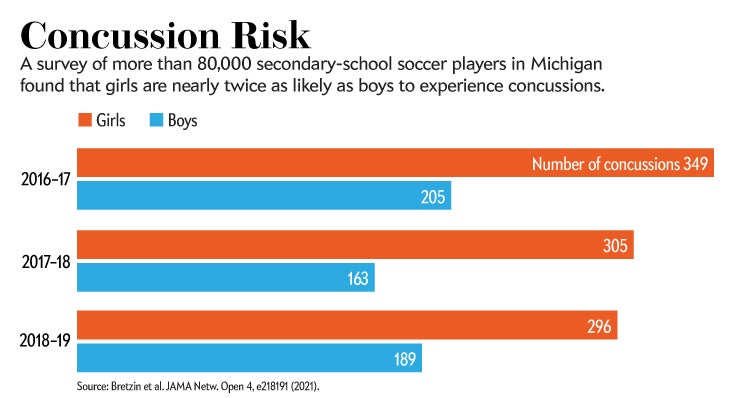
Studies from US collegiate sports have shown that female athletes are 1.9 times more likely to develop a sports-related concussion than are their male contemporaries in comparable sports. Those female students also missed many more study days as they recovered. Neuropathologist Willie Stewart at the University of Glasgow, UK, co-authored a study published earlier this year of more than 80,000 secondary-school soccer players in the United States, with similar results (see ‘Concussion risk’).
It’s not just the number of head injuries that differs between women and men, but also their nature. A review of 25 studies of sport-related concussion suggests that female athletes are not only more susceptible to concussion than are males, but also sustain more-severe concussions.
Athletics trainer and sports scientist Tracey Covassin at Michigan State University in East Lansing was one of the first to look at the differences between the sexes, starting in the early 2000s. She was interested in concussion, but noticed that all the data were coming from male-dominated sports in the United States: ice hockey, boxing and American football. In more than 20 papers over almost two decades, Covassin has shown that there are sex differences in concussion rates and recovery times. In 2013, for instance, she published work on concussed soccer players in the United States, and showed that the female players scored lower in memory tests and experienced more symptoms than did their male contemporaries.
As-yet-unpublished research by Williams on female rugby players—among the first studies to analyse sex-specific mechanisms of head injury in the sport—showed that more than 50% of the 25 female participants experienced injuries caused by their head whiplashing into the ground, whereas only one male player did. “I didn’t expect that. That’s an important discovery,” says Grey, who has seen Williams’s results.
The actions leading to head injuries in female players might also be different. In Stewart’s soccer study, the girls were most likely to injure themselves when they made contact with an object (such as the ball, when heading it for example), whereas the boys were more likely to make contact with another player. Whether this is a matter of coaching, an individual’s level of playing experience or something else isn’t yet known.
Why women fare worse
The damage that causes concussion can be quite subtle. The brain can’t move that much in the skull, explains Stewart. “The brain virtually fills the intercranial cavity, and there’s a little thin film of fluid that fills up what space is left.” But, in the split second after an impact, the head rapidly decelerates, and the resulting forces transmit deep inside the brain. The gelatinous grey matter undergoes significant shear forces when the head stops suddenly, pushing and pulling the brain tissue in a way that can cause structural damage.
And those forces can affect the brains of men and women in profoundly different ways. Doug Smith at the University of Pennsylvania’s Penn Center for Brain Injury and Repair in Philadelphia uncovered evidence that could be crucial for explaining some of the different outcomes seen in women versus men: their brain cells are structurally different.
Every neuron has a major fibre called the axon, which is responsible for transmitting electrical signals from cell to cell. Damage to axons, through strong shear forces, is thought to be the main reason that concussions occur. “Your brain literally can break,” says Smith, holding up some silly putty during a video call to demonstrate. When stretched gently, the silly putty deforms and then relaxes back into shape. When yanked violently, it snaps.
Inside each axon, tiny protein tunnels, called microtubules, that give cells their structure behave similarly, Smith says. These microtubules, only 25 nanometres wide, carry proteins in the axons and help them to function. If a microtubule is damaged, its protein cargo builds up, causing inflammation and ultimately a breakage, explains Smith. “And if you disconnect an axon, it’s gone forever.”
Smith’s team knew from imaging and brain-tissue studies that axon fibres from the brains of female rats and humans are slimmer than those from males. They wanted to know more about the differences and what effect they might have on brain injury, so they cultured rat neurons and then damaged them by exposing them to a rapid air blast. In the neurons from female rats, the axons were smaller and the microtubules narrower and more susceptible to damage than in the cells from males. The same was true for cultured human neurons.
Knowing the extent of axonal damage could be an indicator of how well someone could recover from a concussion. In a sports setting, this could be used to determine when an athlete is safe to return to the field, perhaps in the form of a blood test. Smith is now trying to find biomarkers of axonal damage in the blood—for instance, proteins that leak from axons when they are harmed. He’s doing studies on professional ice-hockey players and measuring axonal protein levels in blood before and after injury. “We did find out that some of these proteins and protein fragments, at a certain level, will actually predict who’s going to have a poor outcome,” says Smith.
Grey urges caution in extrapolating too much from Smith’s work on neurons in culture, which is mainly in rats. “Now that’s not to say that I disagree,” he adds. “It’s just that we need to be cautious. This is one study. I personally think there are other issues that are more important.”
One of those might be differences in neck strength, which some researchers think could have a considerable role in mitigating the damage wrought by concussion. Williams’ mouthguard study also measured neck strength to see what sex differences there are. She found that female players’ necks were 47% weaker than men’s. Williams is working on improving neck strength in female rugby players to understand whether specific training could lessen the likelihood of concussion.

Not everyone agrees, however, that neck strength is the problem, or the answer. Stewart isn’t convinced by any of the studies showing that neck strength is a factor in increasing the risk of a concussion, or a factor in improving the outcome of concussions.
Some researchers, including Grey, favour the idea that concussion is aggravated by the hormones that govern the menstrual cycle.
In 2014, Jeff Bazarian, a physician specializing in brain injury at the University of Rochester Medical Center in New York, published a paper that showed a clear correlation between the menstrual cycle and how women recover from a traumatic brain injury. His team found that women who arrived at the emergency department with a head injury sustained while they were in the luteal phase of the menstrual cycle, which begins after ovulation and is when progesterone levels are highest, fared worse a month later than did women who hit their heads during the follicular stage, which marks the start of a new cycle and ends at ovulation. Women who were taking oral contraceptives, which balance out hormone levels, also fared better.
Initially, this seems counter-intuitive, because progesterone has been shown to have a neuroprotective effect, and the luteal phase is when that hormone peaks. But other studies have reported an association between progesterone and concussion. Martina Anto-Ocrah, a reproductive epidemiologist at the University of Rochester who has continued Bazarian’s work, says this is because the brain injury causes progesterone levels to abruptly plummet.
Anto-Ocrah became interested in concussion and female sexual health after seeing evidence from the US National Football League that some 30 years after sustaining concussions, male athletes were experiencing low testosterone levels and erectile dysfunction. “But there was nothing in the literature for women. I started thinking, why are we not looking at how concussion affects female reproduction, female menstruation, female sexual health?” she says.
Anto-Ocrah is discovering signs that not only does the menstrual cycle have an impact on concussion but, conversely, head injuries can affect the menstrual cycle and other aspects of reproductive function by interfering with the brain regions that, in tandem with other glands in the body, help to control levels of oestrogen and progesterone.
Treating women differently
One thing scientists agree on is the need for more research about women who sustain head injuries. In sports, this could transform the concussion treatment protocols, recovery experiences and the return to play. In July, World Rugby, rugby union’s global governing body, made a statement committing to conduct research into injury-prevention programmes specific to women, and stressing the need for such initiatives. Grey says he knows of no sports bodies that have actually implemented woman-specific concussion measures or protocols.
Research funders are beginning to recognize the need to study sports concussions separately in men and women. The US National Institute of Neurological Disorders and Stroke (NINDS) has allotted a total of US$6.8 million over five years to two large projects studying sex differences in concussion and its assessment.
As part of this push for more data, in 2019, Stewart and his collaborator Katherine Snedaker, who runs PINK Concussions, an advocacy group for women’s head injury, put out a call for more female athletes to pledge their brains to the Glasgow traumatic brain-injury archive he curates. Stewart’s team plans to use the archive to investigate further how traumatic brain injury harms brain tissue and alters gene expression, and how it might go on to cause degenerative brain disease. Of the 1,800 or so donated brains in the archive, 75% are from men; fewer than 200 are from athletes and none of those is from a woman, although a number of high-profile UK-based female athletes have pledged their brains, including Scottish footballer Rose Reilly, judo international Connie Ramsay and Scottish rugby star Lee Cockburn.
Prompted by what she saw on the pitch, and facing some enforced downtime during the COVID-19 pandemic, Williams put together a survey of almost 2,000 female rugby players from 56 countries, who answered questions about their experiences of concussion. Early results suggest that players vary hugely in their knowledge of how to recognize and deal with brain injuries.
Williams says that her work, and that of others, is slowly gaining traction. In April, the University of Otago in Dunedin, New Zealand, announced the start of a study in collaboration with World Rugby that will use a mouthguard to quantify aspects of head injuries in both male and female rugby players.
There are bright spots, but at the moment, Grey says, sports bodies mostly ignore the steadily building knowledge about sex differences in concussion. The male game is still the priority, says Stewart. “There’s this general focus on male sport, male injury and male outcomes, and less on female. It’s terrible neglect.”
This article is reproduced with permission and was first published on August 3 2021.
