Farmworkers in California's Central Valley know that when the tule fog settles over the ground after a heavy rain, some of them are about to get sick. Within a few weeks of the dense fog's arrival, many of the laborers grow tired and develop headaches and fevers. Each time, those who have evaded illness wonder whether they will be next. Experienced farmworkers expect this affliction, but when Rosalinda Guillen arrived from Washington State 25 years ago, she had never seen anything like it. She watched, helpless, as other farmworkers coughed and tried to catch their breath.
That was the first time Guillen, a seasonal farmworker and agricultural justice leader, heard the term “Valley fever.” The disease is caused by two species of shapeshifting fungus in the genus Coccidioides, both of which flourish when exposed to moist springs and arid summers—like those in the San Joaquin Valley, where the fever got its name. Guillen had not encountered such a thing in her home state. But because of drier landscapes and warming temperatures, the fungus's range appears to be spreading.
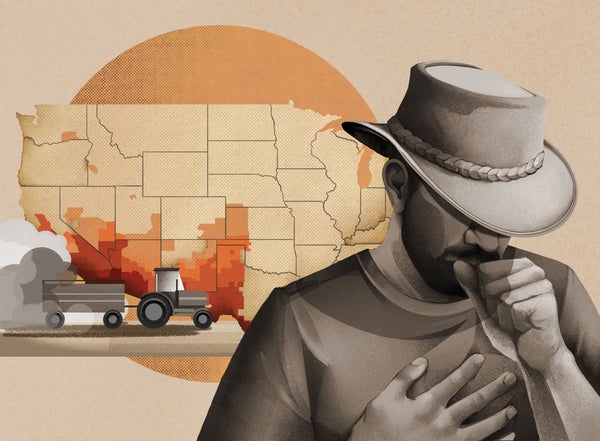
No one knows for sure whether wind is moving Coccidioides north or whether it has been there undisturbed until now. But even as researchers have been discovering it in new pockets throughout the western U.S., many state health departments have failed to track it. What limited data exist indicate that 40 percent of cases become symptomatic, and among those the people most at risk of life-threatening disease are Latino, Asian and Native American people, who contract Valley fever at two to four times the rate of white people. That increased risk seems to be primarily attributable to their frequent exposure and long hours spent in dusty outdoor locations, although genetic variations haven't yet been ruled out.
Many of those affected lack basic health care, and some are afraid to seek medical help for fear of employer retaliation or even deportation. As a result, Valley fever is undersurveilled and underdiagnosed, and its study and treatment are underfunded. Research on the condition has remained limited, but it's clear that the disease disproportionately strikes people in the most vulnerable populations.
After decades of neglect, however, there's a new push at both the local and federal levels to find out more about the extent of Valley fever's threat. In addition, a small group of researchers is working to understand how to treat and even prevent it. That knowledge can't come soon enough, Guillen says: “All we really know is that farmworkers may already be sick.”
Growing Evidence
Valley fever thrives both in dirt and in human lungs. After a heavy rain, the fast-growing Coccidioides spreads through the wet soil like mold through bread. When it dries out, its spores mingle with dusty topsoil and can be inhaled as airborne pathogens. Once they're in the lungs, those spores take on a wholly different form, each morphing into a reproductive cell in which new spores multiply. The full cells burst within five days, releasing spores that travel throughout the body. The fungus can cause coughing, fevers, body aches, fatigue, rashes and appetite loss. In up to 10 percent of those infected, some symptoms can last for years. The Centers for Disease Control and Prevention report that about 200 people die from the disease every year.
Bridget Barker, a mycologist and geneticist at Northern Arizona University, has spent her decades-long career figuring out how to detect Coccidioides and understand its role in the larger ecosystem. She and her team designed a probe to extract it from the soil so they can analyze it. Their research has revealed the fungus's resilience: Coccidioides needs moisture to grow, flourishing when the rains arrive, then stagnating when the ground dries up again. Its spores remain in the topsoil, where they can survive for years.
Barker and others refer to this process as the “grow-and-blow” cycle: once the fungus stops growing and becomes dehydrated, wind picks up the spores and carries them to new areas. This may be one way Coccidioides has expanded into the Pacific Northwest from the southwestern states, such as California, Arizona and New Mexico, where it is endemic. Researchers at the University of California, Irvine, predict that if warming trends continue and droughts persist, Valley fever could eventually stretch as far north as the U.S.-Canada border and as far northeast as North Dakota.
Amanda Gomez-Weaver, a doctoral student in environmental health sciences at the University of California, Berkeley, has been investigating the correlation between climate-influenced dust exposure and Valley fever epidemiology. Previous research had indicated that spores can become airborne anytime dirt is disrupted, making people working in construction and agriculture particularly susceptible. Gomez-Weaver has also found a strong association between Valley fever incidence and ambient dust, indicating that spores become suspended in the air and linger there much like other atmospheric particulates. This work has convinced her that anyone who spends most of their day in dusty outdoor areas in the western U.S. would need a Coccidioides vaccine to remain uninfected. To date, however, no vaccine is available for any fungal disease. A vaccine, Gomez-Weaver says, “would be the most powerful tool in our arsenal.”
The Data GAP
Valley fever's mortality rate is about one death per 1,000 infections, according to infectious disease physician John Galgiani, director of the University of Arizona's Valley Fever Center for Excellence. It doesn't need to be so high. There are medications to treat it, but patients often receive incorrect diagnoses.
Physicians and other health-care practitioners who work where Valley fever is prevalent often don't know to test for it, because there's a general lack of awareness about the disease and because its symptoms can be mistaken for other respiratory illnesses, such as pneumonia. Patients usually end up with antibiotics or other medications that kill bacteria but not fungi.
The CDC estimates that only one in 33 cases is reported and has suggested that hundreds of thousands of infections have probably been missed over the past 10 years. Because the organization does not mandate that public health departments report Valley fever—only 26 states have submitted case numbers—it has no data at all from some states where the fungus is endemic, such as Texas and Idaho.
Farmworkers and laborers who toil in the dusty outdoors, most often people of color, have been trying to get the attention of state and federal agencies for decades. “If something is harming us,” Guillen says, “it's hard to prove based on the way that data-collecting systems are structured.”
Proof of Concept
To show that a vaccine could be effective protection against Coccidioides, Galgiani and his team started by focusing on an immunization for dogs with the infection. Dogs are vulnerable to the disease, too. Because they explore the environment through their noses and can inhale large quantities of fungal spores in a short time, they contract Valley fever more often than humans do, and their symptoms can be more severe.
The canine vaccine Galgiani helped to develop has already proved itself. It uses attenuated live spores of Coccidioides that can't reproduce but still prompt an immune reaction in the body. The response they elicit is so robust that a veterinary pharmaceutical company has licensed the rights to the vaccine and is seeking approval from the Department of Agriculture for its use in pets. Galgiani has now moved on to humans.
One potential benefit of a Valley fever vaccine is that it could be a one-and-done kind of thing—unlike those for influenza or even tetanus, which must be updated regularly. According to studies by microbiologist Deborah Fuller of the University of Washington School of Medicine, people who get Valley fever develop lifelong immunity. That, Fuller says, “is the golden egg.”
Fuller's team is pursuing both DNA- and RNA-based vaccines, each of which would prompt the body to produce proteins that trigger an immune response. Fuller notes that any vaccine against Coccidioides would serve a greater purpose than just fighting Valley fever: it could allow researchers to understand immune response to other fungal diseases and provide insight into how to better treat such conditions.
Galgiani believes that if funding allows, a human version of his vaccine could be ready for approval within eight years. That funding may finally be within reach. After Valley fever's annual incidence surpassed 20,000 cases in 2019, two congressional representatives—Kevin McCarthy of California and David Schweikert of Arizona—called on the National Institutes of Health to make a substantial investment in Valley fever research. Last year the NIH complied, dedicating $4.5 million in funding to the cause.
It's about time, Guillen says. She has seen how agricultural workers are made vulnerable just by the dint of their surroundings, toiling in jobs that expose them to agrochemicals, dehydration, extreme heat, and more. Growing up in Washington State, working in the fields herself starting at age 16, she never had to worry about Valley fever. But now she's watching it creep in and threaten the people she's tried so hard to protect. She's fighting to make sure some of the most invisible workers are seen.
This article is part of “Innovations In: Environmental Health Equity,” an editorially independent special report that was produced with financial support from Takeda Pharmaceuticals.