Inside the gut of a caterpillar lives a worm, and inside the worm lurks a bioluminescent bacterium named Photorhabdus asymbiotica, which makes the caterpillar glow in the dark. But this nesting-doll-like setup has another, more harmful effect: the bacteria secrete a deadly molecular syringe, 100 nanometers long, that latches onto the insect’s cells. Once attached to a cell, the syringe pushes a molecular spear through the cell’s membrane that releases a toxic payload. As its insect host dies and decomposes, the bacteria escape to colonize their next victim.
In a paper published today in Nature, researchers report refashioning Photorhabdus’s syringe—called a contractile injection system—so that it can attach to human cells and inject large proteins into them. The work could provide a way to deliver various therapeutic proteins into any type of cell, including proteins that can “edit” the cell’s DNA. “It’s a very interesting approach,” says Mark Kay, a gene therapy researcher at Stanford University who was not involved in the study. “Where I think it could be very useful is when you want to express proteins that can do genome editing” to correct or knock out a gene that is mutated in a genetic disorder, he says.
The nano injector could provide a critical tool for scientists interested in tweaking genes. “Delivery is probably the biggest unsolved problem for gene editing,” says study investigator Feng Zhang, a molecular biologist at the McGovern Institute for Brain Research at the Massachusetts Institute of Technology and the Broad Institute of M.I.T. and Harvard. Zhang is known for his work developing the gene editing system CRISPR-Cas9. Existing technology can insert the editing machinery “into a few tissues, blood and liver and the eye, but we don’t have a good way to get to anywhere else,” such as the brain, heart, lung or kidney, Zhang says. The syringe technology also holds promise for treating cancer because it can be engineered to attach to receptors on certain cancer cells.
Zhang had been looking for new ways to deliver gene-editing enzymes to cells when, two years ago, he and his graduate student Joseph Kreitz read two papers on Photorhabdus’s injection system. The system was unique because it was adapted to insect cells. “This is one of the very rare examples where a bacterial thing injects into an animal cell,” as opposed to into another bacterial cell, Zhang says. “We thought if this could inject into an animal cell, maybe it could work on human cells.”
The researchers mass-produced the miniature injectors by inserting genetic blueprints for the injectors into Escherichia coli bacteria. The E. coli dutifully secreted the tiny syringes, which, when exposed to insect cells, bound to them and injected their toxins as expected. But when Kreitz and Zhang tested these injectors on human cells, they failed to work. “So then we had to figure out: How do we engineer this thing?” Zhang says.
Zhang’s team homed in on tentaclelike structures on the injectors called tail fibers, which grab and hold onto cells before the injector pierces cells’ membranes. The researchers tweaked these fibers in more than 100 different ways to try to get them to latch on to human cells. Nothing worked. Then, about a year into the project, a newly released version of artificial intelligence software called AlphaFold came to their rescue. AlphaFold predicts the three-dimensional structure of proteins from sequences of amino acids. A 3-D view of a tail fiber protein helped the team figure out how to alter it so that it would reliably attach to human cells.
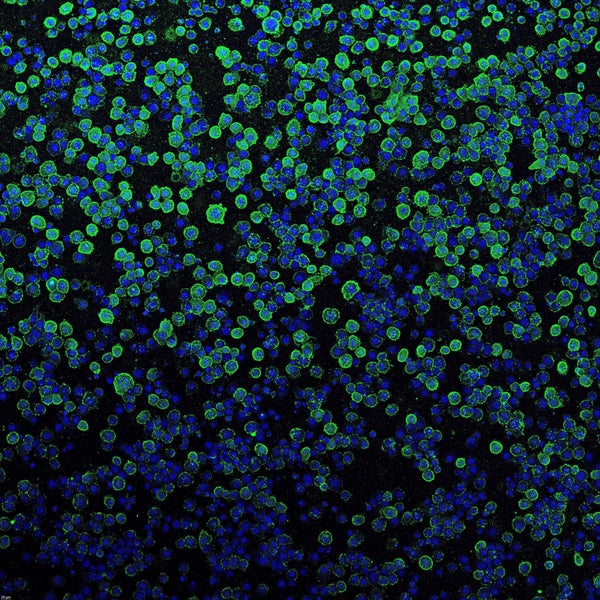
In one experiment, the team was able to make the nanosyringes with altered tail fibers stick to an epidermal growth factor receptor (EGFR) that sits on the surface of some human cancer cells. Loading the injection system with a toxin killed nearly all the cells bearing the receptor but did not harm other cells, illustrating its specificity. The researchers tailored the injectors’ tail fibers to recognize surface markers on other cell types as well.
Zhang’s team also found it could pack the system with various protein payloads by adding a tag to the proteins that marks them as ammunition that needs to be loaded onto a syringe’s needle. The scientists attached this tag to protein toxins and the gene-editing enzyme Cas9, a large molecular scissors that snips DNA at a location specified by a molecule that guides the scissors to the right place. When these proteins were delivered to human cells, they either killed the cells or edited the cells’ genes. “We show that just by putting a tag onto the protein, we can load different types of proteins into these needles,” Zhang says. Each needle also can load multiple copies of a proteins to increase dosage, Zhang says.
To further explore the technology, the researchers again used AlphaFold to engineer these tiny syringes to bind to mouse cells and injected them into the brain of a mouse, where they inserted a protein into neurons that made the cells glow. “Being able to do it intracranially in mice and seeing some delivery of an actual payload in actual neurons—that’s amazing and impressive,” says Rodolphe Barrangou, a geneticist at North Carolina State University who studies CRISPR-Cas but was not involved in the new study.
It is still very early days for the technology, however. Zhang plans to build on its efficiency as a delivery device as well as to experiment with nonprotein payloads such as DNA and RNA. Down the road, it will be important to test the technology in “higher mammals,” Kay says. “There are a lot of things that work well in mice or smaller mammals that don’t end up working as well in nonhuman primates or humans,” he adds. And because the injection systems consist of bacterial proteins, they could also lead to immune reactions in humans. “We need to know: How immunogenic is it if we put it into humans?” Zhang says.
Still, the work showcases the importance of biological inspiration for solving difficult technical problems in biology and medicine, Barrangou says. “This is a very good example of that focus on unearthing from natural biological dark matter items of interest that have practical use and that are good enough to be deployable,” he says.