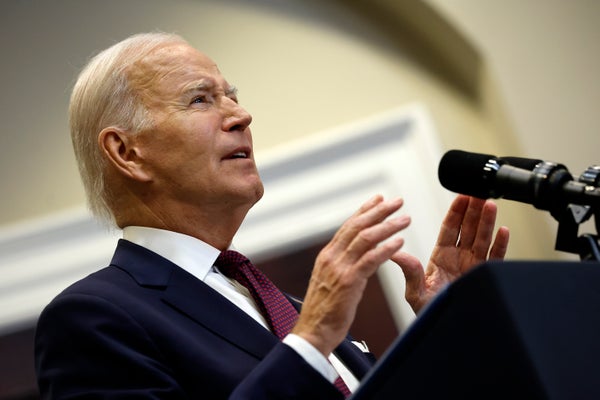
President Joe Biden is using a machine to keep his airways clear while sleeping because he has a condition known as sleep apnea, White House officials say.
Sleep apnea likely affects about 30 million people in the U.S., according to the American Medical Association. Some people with sleep apnea use what’s called a continuous positive airway pressure (CPAP) machine, which includes a mask that a user straps onto their face at night to breathe better while they sleep.
Officials revealed Biden has been using a CPAP machine after reporters recognized indentations on his face from the strap holding the device in place. Documents released as early as 2008 show Biden has been known to experience sleep apnea, which can become more common as people age.
Scientific American spoke with Christine Won, medical director of the Yale Centers for Sleep Medicine, about sleep apnea, its causes and treatment with CPAP machines.
[An edited transcript of the interview follows.]
What is sleep apnea?
Obstructive sleep apnea occurs because there’s a problem with the structure or the function of the upper airway. When we fall asleep, the upper airway loses its muscle tone, and if your airway is narrow, this might lead to obstruction. This can cause people to snore, or it can also completely obstruct the airway and cause people to not be able to ventilate well. This can lead to low oxygen levels; it can lead to disturbances in sleep. People can sometimes awake abruptly as a result, and sleep is fragmented.
Are there different kinds of sleep apnea?
Yes, [in addition to obstructive sleep apnea, there is a type called] central sleep apnea, which is far less common. It generally affects older men and people with heart disease, although it can be found sometimes in healthy individuals. This type of sleep apnea results from the brain not communicating during sleep to the respiratory muscles to take a breath, and so there are pauses in breathing.
What are the symptoms of sleep apnea?
Both types of sleep apnea can disrupt sleep because the person may awake abruptly because they’re not getting enough oxygen. Snoring comes more with the obstructive sleep apnea. And then both types, because they can disturb sleep, can lead to daytime symptoms such as sleepiness or brain fog, these types of things.
How common is sleep apnea?
Sleep apnea is very common in the adult population. Prevalence increases with weight gain—so it’s much more prevalent in individuals with obesity. It’s more common as we age. It’s also twice as common in men as in women, for unclear reasons.
There are a lot of people who have sleep apnea that are undiagnosed. I think current data suggest only about 20 percent of people with sleep apnea are actually diagnosed.
Why do you think so many people go undiagnosed?
Probably a little bit of education—not knowing what the symptoms of sleep apnea are, not knowing that waking up a lot at night, unrefreshing sleep, these types of things can be a sign of sleep apnea and not just, “normal.” There might be a little bit of resistance to undergo a sleep study, and maybe there might be a little bit of resistance in accepting CPAP as a form of therapy for this.
What causes sleep apnea?
The structure problem is that the airway can be narrowed for various reasons. There could be excessive fat in the neck tissues. The soft palate could be redundant and low-hanging and basically blocking the airway. The tongue base could be very big and bulky, again, reducing the airway size. Some people can have very large tonsils and adenoids [lymphatic tissue near the tonsils] that can obstruct the airway. Also, the jaw anatomy can affect the airway size—people who have really small jaws or recessed jaws, their airway can be narrowed.
And some people can have very wide, open airways while they’re awake, and they don’t have any of those anatomical issues that I just described. But when they fall asleep, airway muscle tone decreases markedly and can lead to airway collapse. It’s not clear why. But the upper airway is basically a large muscular tube: it’s not supported by bony structures, so muscle tone is important to keep the integrity of the airway. That may be why aging is related to increased risk of sleep apnea, because with aging, all our muscles get a little bit more relaxed.
What are common treatments for sleep apnea?
CPAP is the most common treatment for sleep apnea because it’s highly efficacious—so in other words, if you wear it, almost always it’s going to eliminate obstructive sleep apnea. The problem is that a lot of people have difficulty tolerating CPAP, so it’s not an effective treatment for everyone.
Other treatments include oral appliances that you get fitted for by your dentist. You fit the appliance into your mouth at night, and it pulls your lower jaw forward so the airway doesn’t collapse while you’re sleeping. That’s a reasonable treatment option for people who are young and thin and generally have mild sleep apnea.
There are also a lot of surgeries, such as a maxillomandibular advancement surgery, which is a pretty big surgery where they cut your jaw and advance it—up to a centimeter sometimes—to open up the airway in the back. Tonsillectomy and adenoidectomy are actually mainstay treatments for children with sleep apnea—generally not for adults.
A newer form of therapy is upper airway stimulation. It’s like a pacemaker for the tongue, essentially. But it’s not a therapy for everyone—there are specific criteria and a specific population who would benefit from that.
And not all sleep apnea needs to be treated. We know that sleep apnea is associated with cardiovascular disease and risks. What we don’t know is how much CPAP therapy benefits [people or who will benefit from it]. So even if you’re diagnosed with sleep apnea, it doesn’t automatically mean that you go to CPAP therapy. You’d have a discussion with your doctor about [questions such as] “How symptomatic are you? What kind of cardiovascular risks do you have? How severe is your sleep apnea?” Based on these things, your doctor will decide if you would benefit from treatment or not.
How do CPAP machines work?
They’re basically reverse vacuum cleaners. They have a motor that generates positive pressure that’s transmitted via a tube and a mask into the pharyngeal space. And it acts like a pneumatic splint, and it just holds open the airway, so it doesn’t collapse.
How easy is it to get a CPAP machine?
They’re very accessible: if you’re diagnosed with sleep apnea, and you meet specific criteria from an insurance perspective, then it’s easy to prescribe and obtain one.
It is somewhat difficult for patients to keep their CPAP or get renewed supplies, because for insurance, you sometimes have to meet these metrics of using it at least four hours a night for 70 percent of nights for 30 days consecutively. It’s kind of tough because a lot of people don’t take to CPAP right away. Some people do—like first night, they love it; it’s the best sleep of their life. But other people, it takes some time to get used to it, because this machine on your face is blowing pressure. It’s a foreign sensation.
What should people do if they think they might have sleep apnea?
They should definitely discuss it with their doctor, who can further screen and evaluate their symptoms and decide if they are at risk for it and then refer them for a sleep study.